The Role of AI in Healthcare: Use Cases, Challenges and Future Outcomes
The role of artificial intelligence (AI) in healthcare is groundbreaking. It is revolutionizing the doctor-patient relationship and providing smarter ways to diagnose, treat, and monitor patients.
According to research published in Academic Radiology, the AI model can help detect breast cancer on MRI scans a year earlier than current methods. This is just one of many applications AI is advancing in healthcare.
Integrating AI into healthcare promises significant benefits in disease diagnosis, treatment decisions, and laboratory testing. Additionally, it has the potential to save $360 billion annually in the healthcare industry.
Considering all aspects, we have created this comprehensive guide to help you understand the role of AI in healthcare. We will explore its basics, use cases, challenges, case studies, and future prospects.
For a comprehensive coverage of this topic, please read the book titled” Transforming Healthcare: The Role and Impact of Artificial Intelligence.”
What is AI in Healthcare?
AI in healthcare involves applying AI technologies to various healthcare tasks, including:
- Analyzing complex medical data
- Assisting in disease detection
- Personalizing treatment plans
- Streamlining administrative processes
- Improving patient care
- And many more.
AI can enhance nearly every aspect of the healthcare sector through its various advanced technologies. The primary AI technologies employed in healthcare include:
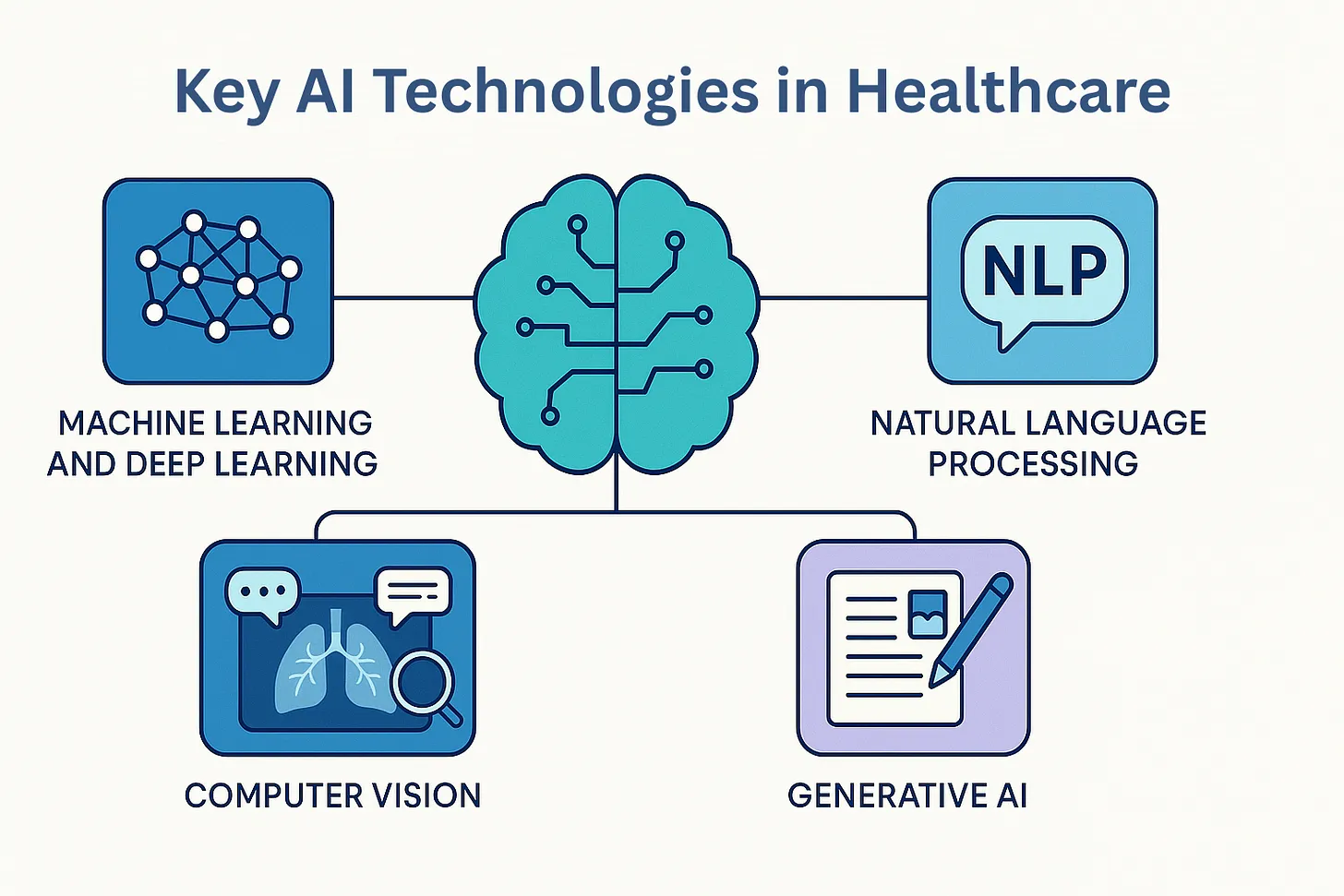
1. Machine Learning and Deep Learning
Machine learning (ML) and deep learning are central to AI’s transformative influence on healthcare. ML algorithms process large datasets, such as electronic health records, imaging, and genomics. They uncover hidden patterns, make predictions, and aid clinical decisions.
Deep learning is a subset of ML that utilizes neural networks with multiple layers and excels at complex tasks, such as medical image analysis, early disease detection, and risk stratification.
ML and deep learning technologies enable personalized medicine. They tailor treatments to individual genetic profiles and medical histories. Additionally, they keep learning from new data to boost diagnostic accuracy and improve patient outcomes.
2. Natural Language Processing
Natural Language Processing (NLP) is a specialized area of AI focused on helping machines understand, analyze, and produce human language from unstructured clinical texts. These processes use algorithms like tokenization, named entity recognition, and syntactic parsing to turn free-text physician notes, discharge summaries, and pathology reports into organized data.
There are now transformer-based architectures (GPT, BERT, etc.) that provide contextual understanding and semantic analysis. They support tasks such as automated clinical documentation, extracting comorbidities, and identifying adverse drug events.
NLP also enables chatbots and virtual assistants to answer patient questions, schedule appointments, and handle other tasks. In short, NLP decreases administrative workload through better data sharing and supports real-time clinical decision-making.
3. Computer Vision
Computer vision uses advanced image processing and pattern recognition algorithms to analyze visual data from medical imaging methods. These include X-rays, CT scans, MRIs, and digital pathology.
Computer vision systems are trained on large annotated datasets to detect subtle abnormalities, such as early-stage tumors or microscopic tissue changes, that the human eye might overlook.
Besides diagnostics, computer vision helps with image-guided procedures, tracks disease changes, and more. Today, it is increasingly integrated into radiology and pathology workflows to lower diagnostic mistakes, speed up reporting, and enhance clinical skills.
4. Generative AI
Generative AI refers to models that can produce new content, like text, images, or even synthetic medical data. They generate content based on learned patterns from existing data.
Generative AI in healthcare is used to simulate patient scenarios, create synthetic datasets for research while protecting privacy, and develop personalized patient educational materials. It also helps in drug discovery by designing new molecular structures and predicting drug interactions.
Generative AI assists clinicians by drafting patient summaries, clinical notes, and reports. This significantly reduces administrative workload. In short, the ability to generate context-aware content allows generative AI to accelerate innovation, support research, and improve patient engagement. In fact, 92% of healthcare leaders believe generative AI improves operational efficiency, and 65% see it as a valuable tool for speeding up decision-making.
Evolution of AI in Healthcare?
Several factors contributed to the integration of AI into healthcare. However, the root of this evolution lies in decades of foundational research in computer science and artificial intelligence.
The development of AI in healthcare dates back to the 1950s and 1960s. During that period, pioneers like John McCarthy and Marvin Minsky laid the foundation with the principles of symbolic reasoning and problem-solving.
The 1970s saw the rise of expert systems like Dendral and MYCIN at Stanford. These systems used rule-based logic to help with molecular structure analysis and infectious disease diagnosis. Although these systems performed similarly to experts in specific areas, their limited adaptability and dependence on manual rule encoding hindered widespread use.
The 1980s and 1990s marked a shift toward machine learning. Support vector machines, early neural networks, and other algorithms were being applied to medical imaging. Computer-aided detection (CAD) systems started to support radiologists in spotting abnormalities. This period showed that algorithms could learn from data, surpassing static rules.
The 21st century marked the beginning of the big data and deep learning era. Digitization of health records, improvements in processor speed, and the emergence of next-generation genomic sequencing allowed AI to analyze large and complex datasets.

Deep neural networks now drive diagnostic imaging, risk prediction, and precision medicine. They combine multi-modal data from genomics, wearables, and electronic health records. As a result, AI has shifted from rule-based systems to adaptive, data-driven platforms capable of transforming every part of modern healthcare.
Use Cases of AI in Healthcare
AI has transformative power in the healthcare industry. It provides a wide range of applications to support various healthcare activities. Some of the common use cases of AI in healthcare include:
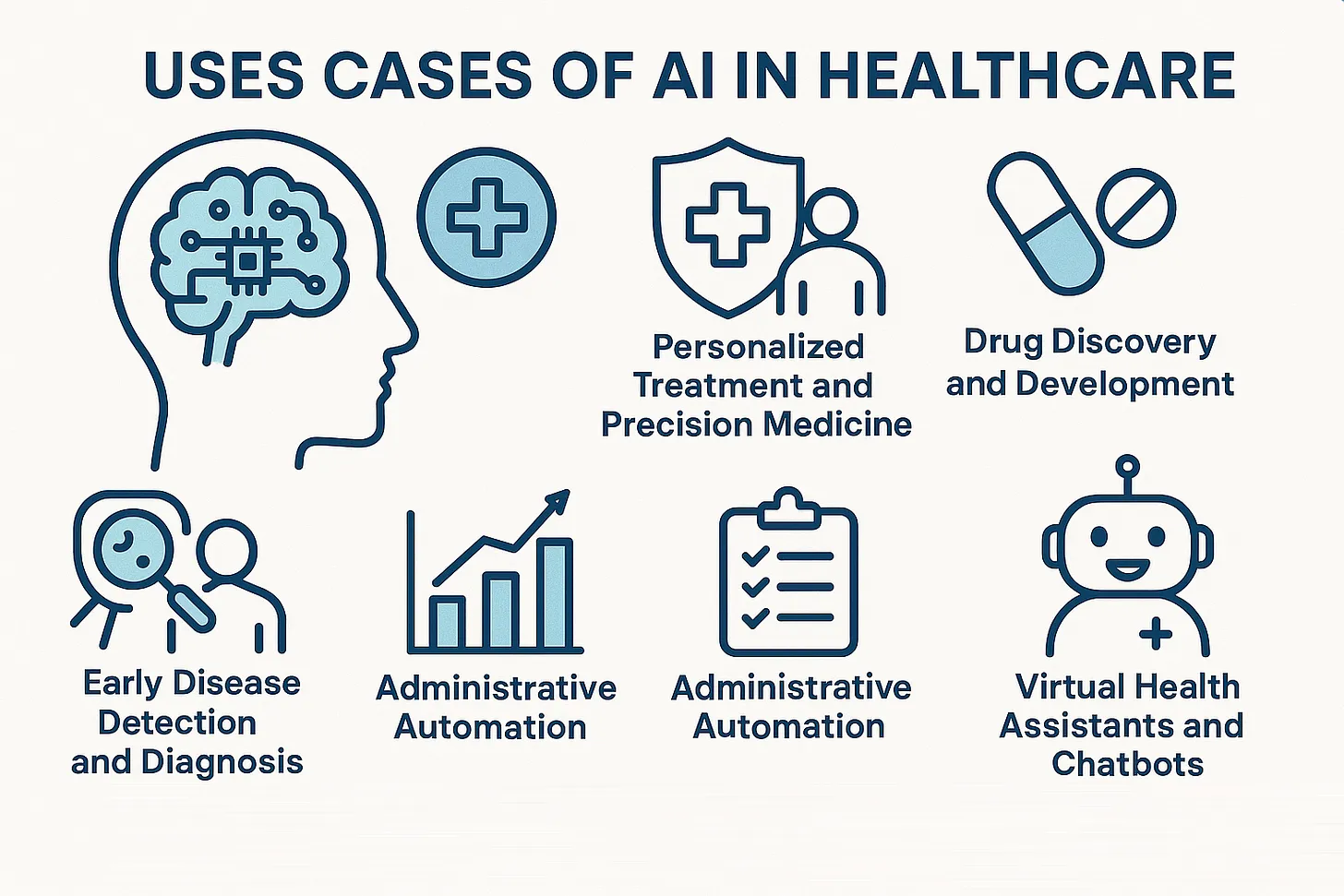
1. Early Disease Detection and Diagnosis
AI is becoming a crucial technology for analyzing medical images, such as X-rays, MRIs, and CT scans. It allows for earlier and more precise detection of diseases like cancer, tuberculosis, and neurological disorders.
Machine learning models can detect subtle patterns that human clinicians might overlook. They assist with earlier interventions and higher survival rates. For instance, a prospective multicenter cohort study in South Korea found that AI-based computer-aided detection increased cancer detection rates by 13.8% compared to radiologists alone.
2. Personalized Treatment and Precision Medicine
AI systems assist in creating personalized treatment plans by combining genomic data, electronic health records, and real-time patient monitoring. These systems can suggest the best drug combinations, modify dosages, and forecast adverse reactions.
Machine learning models analyze large datasets containing patient histories, genetic markers, and treatment outcomes. They identify correlations between specific genetic variants and drug responses, and then AI recommends optimal therapies and dosages. This personalized approach reduces side effects and improves treatment effectiveness.
3. Drug Discovery and Development
AI is also speeding up the drug discovery process. It helps predict molecular interactions, simulate drug-target binding, and identify promising compounds.
Basically, AI platforms use algorithms like generative adversarial networks (GANs) and deep learning to analyze chemical structures and biological data. These systems predict which molecules are most likely to effectively interact with disease targets. Virtual screening and in silico simulations replace some laboratory experiments. This reduces the time and cost necessary to bring new therapies to market.
Pharmaceutical companies now use AI to quickly screen billions of molecules. This makes the preclinical phase more efficient and boosts the chances of finding successful drug candidates.
4. Remote Monitoring and Telemedicine
AI-powered wearables and IoT sensors allow continuous remote monitoring for patients with chronic conditions. AI processes real-time data to identify anomalies, forecast health declines, and notify care teams quickly.
For example, a 54-year-old man in the U.S. was rescued after his Apple Watch repeatedly alerted him to an abnormal heart rate. Medical tests uncovered a severe heart blockage, leading to surgery and the implantation of a pacemaker.
In the background, wearable devices gather real-time data such as heart rate, glucose levels, and more. AI algorithms evaluate this data to identify anomalies or trends that could indicate health issues. When risk limits are exceeded, the system notifies healthcare providers or patients.
5. Administrative Automation
Natural language processing and AI-powered automation are revolutionizing healthcare administration. These technologies gather data from clinical notes, automate coding and billing processes, and make appointment scheduling more efficient.
AI reduces paperwork and administrative tasks, allowing healthcare professionals to concentrate more on patient care. Additionally, AI-powered digital assistants handle patient inquiries and reminders, further increasing efficiency.
6. Predictive Analytics for Population Health
AI models analyze large-scale health data to identify at-risk populations, forecast disease outbreaks, and guide public health strategies. Machine learning models detect trends and risk factors that might not be obvious through traditional analysis.
The insights assist healthcare organizations in targeting interventions and allocating resources more effectively. For instance, predictive analytics helped healthcare systems efficiently allocate resources during the COVID-19 pandemic.
7. Virtual Health Assistants and Chatbots
AI-powered chatbots and virtual assistants offer patients 24/7 access to medical information, appointment scheduling, medication reminders, and symptom triage. They have become frontline virtual helpers for patients. This not only enhances patient engagement but also lessens the workload on clinical staff.
NLP allows chatbots to understand and respond to patient questions naturally. These systems access integrated health databases to deliver accurate information and guidance. AI can assess symptoms, guide patients to proper care, and handle routine tasks automatically. The assistants keep improving through user feedback and interactions.
8. Clinical Trial Optimization
AI streamlines patient recruitment for clinical trials. It matches eligible candidates from extensive health databases using ML, which boosts enrollment efficiency and diversity. AI also monitors trial data in real time to detect safety signals and improve study protocols
Risks and Challenges of AI Implementation in Healthcare
The implementation of AI in healthcare is essential, but it is not without risks and challenges. It is vital to manage these complications for safer and more effective AI deployment.
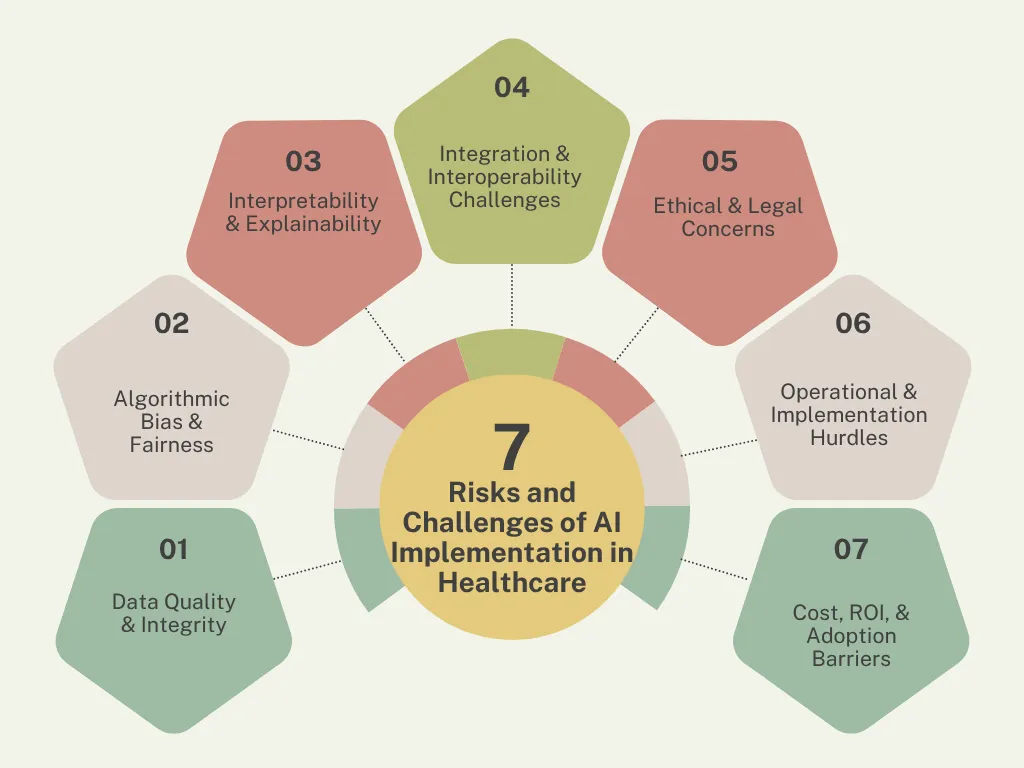
Data Quality & Integrity
The effectiveness of AI in healthcare depends on having accurate, current, and complete data. Poor data quality can undermine the reliability of AI results, which can affect clinical decisions and patient care.
Some of the typical challenges related to data quality include:
- Incomplete or missing patient records
- Incorrectly annotated medical images or clinical notes
- Inconsistent data formats across systems
- Outdated or erroneous information
- Lack of standardized data collection
Data quality issues can be fixed if the healthcare provider sets up a strong data governance framework and consistent data validation measures.
Algorithmic Bias & Fairness
Bias in AI algorithms can cause unequal healthcare outcomes, especially for underrepresented or vulnerable groups. This issue often results from unbalanced or non-representative training data. For instance, an AI model trained on Caucasian skin images experienced a 30% drop in melanoma detection accuracy for patients with darker skin tones.
The common challenges include the following:
- Underrepresentation of minorities in datasets
- Historical biases embedded in records
- Disparities in model performance across groups
- Limited transparency in bias detection
Using diverse datasets and regularly auditing models for bias can help promote fairness and equity in AI applications.
Interpretability & Explainability
Many advanced AI models, especially deep learning systems, are often called “black boxes,” which makes it hard for clinicians to understand how decisions are made.
The lack of transparency can limit trust and adoption. For example, an AI system flagged a lung nodule as suspicious on the chest CT scan. However, it failed to explain why it was concerning.
Developers should prioritize explainable AI techniques to improve interpretability. Engaging clinicians in designing and validating AI tools can help connect technical complexity with clinical usability.
Integration & Interoperability Challenges
Often, integrating AI into existing healthcare systems is difficult due to fragmented IT infrastructures and a lack of interoperability between platforms. For example, an AI system meant to predict sepsis in the ICU failed to send timely alerts because it relied on outdated HL7 protocols, which couldn’t connect with the hospital’s newer FHIR-based monitoring system. This technical mismatch forced staff to manually check patient data.
The common challenges include:
- Disparate EHR systems and data silos
- Legacy software restricts compatibility.
- Workflow disruptions from poor integration
- Lack of industry-wide standards
Using standardized terminology (SNOMED-CT, LOINC), conducting thorough compatibility tests, and involving IT and clinical teams can reduce these challenges.
Ethical & Legal Concerns
AI in healthcare raises important ethical and legal questions, particularly about consent, accountability, and patient rights.
Healthcare services face various regulatory compliance challenges, including HIPAA, SaMD, GDPR, and others. For example, HealthNet was fined $2.5 million for violating HIPAA after patient data was exposed through an unencrypted AI analytics system.
The other challenges include:
- Unclear liability in cases of AI-driven errors or harm
- Informed consent may be lacking for AI-based interventions
- Potential for misuse or unauthorized secondary use of patient data
- Balancing automation with the need for human oversight
Clear guidelines for consent, accountability, and oversight must be established and kept current. Additionally, involving ethicists, legal experts, and patient advocates in AI governance helps ensure responsible deployment.
Operational & Implementation Hurdles
Handling operational challenges when shifting AI from pilot projects to routine clinical use requires significant effort. Resistance to change and unpreparedness can hinder adoption. For instance, a mid-sized hospital invested $800,000 in an AI radiology system, yet after six months, usage stayed below 30%.
The typical operational challenges include:
- Workflow disruption
- Alert fatigue
- Training gaps
- Technical support deficits
- Resistance to change
Comprehensive training programs, clear communication about AI’s benefits, and involving end-users early in the process can increase acceptance.
Cost, ROI, & Adoption Barriers
The financial investment needed for AI implementation can be substantial. For instance, technology licensing and maintenance costs can range from $100,000 to $2 million annually. Additionally, demonstrating a clear return on investment (ROI) is often difficult, especially for smaller organizations.
The common challenges include:
- High upfront costs for technology, infrastructure, and training
- Uncertainty about long-term savings or efficiency gains
- Difficulty quantifying the value of improved outcomes or workflows
- Budget constraints in resource-limited settings
Healthcare leaders should perform thorough cost-benefit analyses and pursue external funding or partnerships when possible. Additionally, demonstrating early wins and measurable improvements in patient care or efficiency can help justify investments and promote broader adoption.
Case Studies of AI in Healthcare
Numerous case studies show the transformative impact of AI in healthcare. Let’s examine two case studies to understand AI’s influence:
Case Study 1: Community Hospital – Streamlining Workflow with AI
A 200-bed community hospital serving 150,000 people faced long emergency department (ED) wait times (an average of four hours) and stagnant patient satisfaction scores of 78%. The hospital also had limited IT resources and staff, which emphasized the need for an affordable way to enhance patient flow and operational efficiency.
The hospital implemented an affordable Natural Language Processing (NLP) platform to tackle this challenge. The system automatically reviewed triage notes to identify high-risk patients, resulting in better prioritization and resource distribution in the ED.
Outcomes:
- ED efficiency increased by 15%.
- Average patient wait time reduced from 4 hours to 3 hours.
- Patient satisfaction scores rose from 78% to 89% over six months.
- Nursing staff experienced a 20% decrease in administrative workload.
Key to success were a user-friendly interface, strong vendor support, and hands-on training to encourage staff buy-in.
Case Study 2: Pharma Partnership – Accelerating Drug Discovery with AI
A pharmaceutical company faced long drug discovery cycles. It often took up to 18 months to identify promising lead compounds. Pressured to develop innovative treatments faster, the company sought a way to accelerate early-stage drug development while maintaining safety and efficacy.
The company partnered with an AI biotech firm to develop a deep learning model that integrated molecular docking simulations and reinforcement learning. This combined AI approach prioritized compounds most likely to bind to target proteins. It sped up the screening process and improved efficiency.
Outcomes:
- Lead compound identification time reduced from 18 months to 6 months.
- Three candidates advanced to Phase I clinical trials.
- Early-stage R&D costs decreased by 35%.
- Compound success rate in preclinical testing improved from 12% to 28%.
The key to success was clear data-sharing agreements, multidisciplinary teams, iterative model validation, and strong executive support from both organizations.
The Regulatory Landscape of Healthcare with AI
The integration of AI into healthcare is carefully regulated to ensure patient safety and effectiveness. In the United States, the Food and Drug Administration (FDA) oversees this process. It reviews AI-based medical devices and software through its Center for Devices and Radiological Health (CDRH).
The FDA classifies AI tools by risk levels (Class I, II, III), with Class I devices considered low-risk, Class II as moderate-risk, and Class III requiring a thorough FDA review. Most AI diagnostics are categorized under Class II and need substantial evidence of safety and effectiveness through pathways like 510(k) or De Novo submissions.
Some of the key regulatory focus areas for using AI in healthcare include:
- Pre-Market Review: AI tools must undergo rigorous clinical validation, with prospective studies preferred for stronger evidence. Submissions must include data on sensitivity, specificity, and performance across diverse patient groups.
- Algorithm Transparency: Regulators demand explainable AI, such as heat maps or confidence scores, and clear labeling of intended use, limitations, and target populations.
- Post-Market Surveillance: Approval is not the final step. Manufacturers must continuously monitor AI performance, report adverse events, and address model drift as patient populations and clinical practices change.
- Data Privacy: Adhering to HIPAA (US) and GDPR (EU) is crucial. This involves de-identifying patient data, obtaining consent, and implementing strong data protection measures, such as encryption and access controls.
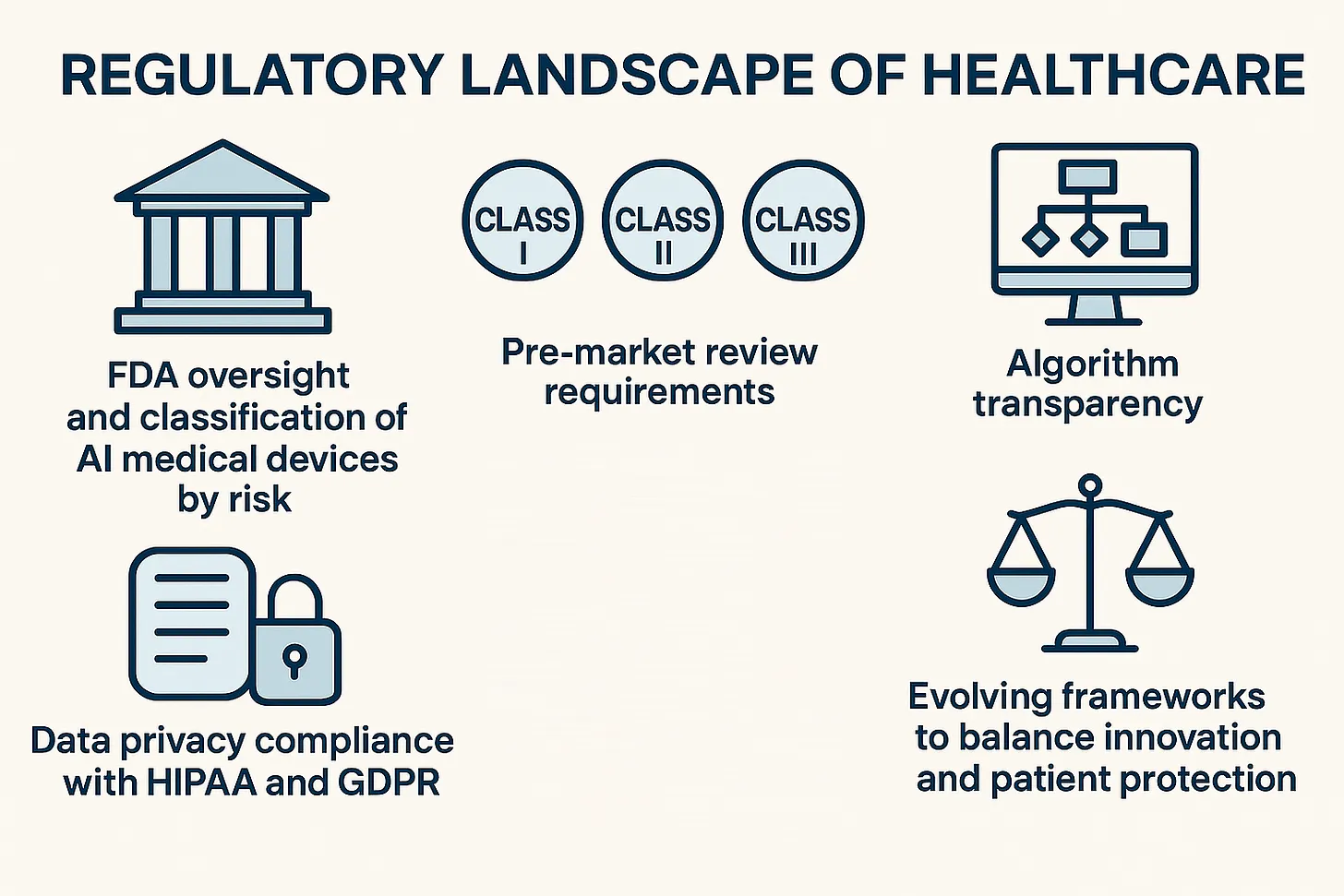
The regulatory landscape is changing to keep up with innovation. The success of AI in healthcare depends on early interaction with regulators, clear clinical evidence, and a continuous focus on safety and fairness.
In short, regulatory frameworks will continue to evolve as AI technologies develop, striking a balance between innovation and patient safety.
Final Words: What’s Next for AI in Healthcare
AI’s expanding use cases are driving a paradigm shift in healthcare. It is making care more proactive, personalized, and accessible than ever before. However, what we are seeing right now is just the beginning of AI’s contribution to the healthcare sector.
The next wave of AI will go beyond hospital walls and democratize advanced diagnostics and treatment for every community. Some of the emerging trends worth catching include:
- Federated and Edge Learning: Allowing global collaboration on AI models while preserving patient privacy and enabling real-time analysis in remote settings.
- Next-Generation Models: Vision Transformers and Graph Neural Networks are pushing diagnostic accuracy to new heights, while multimodal AI combines imaging, genomics, and health records for holistic care.
- Democratization & Equity: Affordable and smartphone-based AI and open-source models are making advanced care possible even in underserved regions.
- Precision Public Health: AI-driven analytics now predict outbreaks, optimize resource allocation, and target preventive care for at-risk populations.
To conclude, the future of AI in healthcare offers improved quality, equity, and accessibility. However, it also relies on responsible innovation, ethical deployment, and workforce preparedness to ensure these powerful tools are used effectively.
Learn more about how TechCon Global is shaping the future of healthcare innovation and AI at their upcoming events, where industry leaders and experts come together to explore cutting-edge technologies and their impact on the healthcare sector.




